Read time: 7 minutes
- Living with diabetes puts you at a higher risk of depression compared to people who don’t live with the chronic condition.
- While antidepressants can help treat symptoms of depression and other mental health concerns, they can also come with side effects that make it more difficult to manage diabetes, from fluctuations in weight to impaired glycemic control.
- Despite these possible side effects, antidepressants can still be part of a healthy diabetes self-care plan.
When you live with diabetes, you’re two to three times more likely to experience depression compared to people without the condition. Whether your mental health has taken a hit because of the day-to-day challenges of managing your blood sugar, or you’re going through a rough time outside of your diabetes management, you and your doctor might decide that it’s best for you to take antidepressants. But what kinds of effects can antidepressants have on your diabetes management?
Defining Different Antidepressants and Their Effects On Your Health
First, let’s be clear about what antidepressants are and how they work. According to the Mayo Clinic, antidepressants are medications that can help reduce symptoms of depression, anxiety, and similar mental health issues. Generally speaking, antidepressants can help treat symptoms by affecting neurotransmitters (chemicals that assist with communication between brain cells) that are associated with these conditions, including serotonin, norepinephrine, and dopamine.
Selective serotonin reuptake inhibitors (SSRIs) including Prozac, Paxil, Zoloft, or Lexapro, increase serotonin levels in the brain and block the reabsorption (or reuptake) of serotonin into neurons, making the neurotransmitter more available in the brain, thus improving communication between brain cells. Serotonin and norepinephrine reuptake inhibitors (SNRIs), on the other hand (Cymbalta, Effexor XR, Fetzima), block the reuptake of both serotonin and norepinephrine to make both neurotransmitters more available and efficient in the brain. Tricyclic (or cyclic) antidepressants (Tofranil, Pamelor, Norpramin) also work by blocking the reabsorption of serotonin and norepinephrine, in addition to other chemical messengers in the brain related to mood regulation and depression. Then there are monoamine oxidase inhibitors (MAOIs) such as Parnate, Nardil, and Marplan, which target an enzyme called monoamine oxidase that’s involved in removing norepinephrine, serotonin, and dopamine from the brain. MAOIs help prevent that removal process, making those brain chemicals more available to regulate mood and depressive symptoms.
Other common antidepressants that don’t fit into the above categories include trazodone (Desyrel, Oleptro), mirtazapine (Remeron), vortioxetine (Trintellix), vilazodone (Viibyrd), and bupropion (Wellbutrin). Some treatment regimens also call for combinations of different antidepressants, depending on the circumstances.
So, how can these different antidepressants affect diabetes management?
1. Antidepressants and Weight
“One of the largest connections between diabetes and antidepressant use seems to be increased weight gain,” says Lisa Graham, a registered nurse (RN), certified diabetes care and education specialist (CDCES), and director of clinical operations at One Drop. Although some types of antidepressants have been associated with weight loss or no change in weight, many do have a possible side effect of weight gain. It’s worth noting that not everyone experiences these side effects and that antidepressants aren’t always a direct cause of changes in weight.
Think about it this way: If you’re taking an antidepressant that increases serotonin in your brain, that means you’re improving several functions in your body that are affected by that neurotransmitter, explains Graham, including your appetite. A better appetite might lead to increased weight gain, which, in turn, can increase insulin resistance, potentially leading to not just weight gain, but effects on blood sugar, too. In that case, antidepressants are doing what they’re supposed to do; they just happen to come with an unintended side effect.
Still, it’s understandable to be concerned about potential changes in your weight when you’re already managing a chronic condition that can easily be complicated by those shifts. That’s why it’s crucial to talk to your doctor about the right treatment regimen for you and ensure that you’re addressing both your mental and physical health needs.
RELATED CONTENT
What It Takes to Manage Your Weight When Living with Insulin Resistance
2. Antidepressants and Blood Sugar
When it comes to antidepressants’ potential impacts on blood sugar, the research is pretty mixed. Some studies have found that noradrenergic (those that only increase norepinephrine in the brain) antidepressants and SSRIs can both impair glucose tolerance and worsen glycemic control in people living with diabetes. Other studies will tell you that SSRIs, along with MAOIs, actually improve glucose homeostasis. Some research argues that these effects are highly dependent on both dose and duration of antidepressant use, making it difficult to generalize to large populations.
Translation: We need more research on the link between antidepressants and blood sugar before we can definitively say the two share a strong relationship in one way or another.
Still, there’s also something to be said about antidepressants’ potential indirect effects on blood sugar via the side effects that can come with the medication—including not just effects on weight, but also drowsiness, fatigue, sexual dysfunction, and agitation, all of which might lead to increased stress levels that can then make it difficult to manage your blood sugar levels, explains Graham.
With all of that in mind, considering some people do see changes in their blood sugar levels with antidepressant use, it’s worth having an open conversation with your doctor, and maybe even your One Drop coach, about how to balance the pros and cons.
3. Antidepressants and Heart Health
Reminder: Living with diabetes puts you at a higher risk of heart disease and other cardiovascular issues, so it’s important to be aware of your heart health when managing diabetes, regardless of whether you take antidepressants.
That said, much like antidepressants’ possible effects on blood sugar, it’s unclear how these medications impact heart health. Some research will tell you that heart-related concerns like hypertension (high blood pressure) and tachycardia (a condition that makes your heart beat too fast) have been reported with certain antidepressants; other studies show that some antidepressants, such as SSRIs, may actually be associated with a reduced risk of myocardial infarction (heart attack) in some populations, including in people with diabetes.
Plus, as Graham notes, the weight gain associated with antidepressants can exacerbate the risk of obesity, which can worsen cardiovascular health in addition to complicating diabetes management.
“Especially if you have existing heart disease, high blood pressure, and/or high cholesterol, it’s important that you monitor these factors closely,” says Graham. And, even if you don’t currently live with any of these conditions, she stresses, talk with your doctor about monitoring these levels regardless while you’re being treated with antidepressants.
RELATED CONTENT
Why Heart Health Is a Necessary Part of Your Diabetes Self-Care
Antidepressants Aren’t the Only Culprit, Though
Antidepressants may have unique effects on different aspects of metabolic health, but we can’t talk about those effects without acknowledging the role of depression itself as well.
As Graham says: “When we don’t feel well mentally, we may not pay attention to our health.”
You’ve been there: When you live with a chronic condition like diabetes, it can already be exhausting and debilitating to keep up with your day-to-day (sometimes even moment-to-moment) blood sugar levels and the countless factors that can influence them—from the ones that are within your control to the ones that aren’t. Research shows that the burnout of managing diabetes commonly leads to what’s known as diabetes distress, or the feeling of being overwhelmed by the burden of diabetes management.
If left untreated, diabetes distress can eventually develop into depression—and depression itself can lead to either weight gain or weight loss, which could have an effect on your diabetes management, notes Dr. Markus Ploesser, MD, a board-certified psychiatrist, integrative physician, and chief innovation officer at Open Mind Health.
You might be thinking: Isn’t that what antidepressants are for, though? The short answer is yes, but the reality is that antidepressants don’t always work to treat depression—at least, not always right away, and not always for the long term. It can take time to figure out the right type of medication for your body, not to mention the dose and duration, and in the meantime, you might continue noticing certain effects that your mental health has on your diabetes management, irrespective of antidepressants, whether it’s a hormonal imbalance caused by depression or a fluctuation in your weight caused by lack of appetite or emotional eating.
The Bottom Line
Put simply: “Living with diabetes will influence your choice of antidepressant,” says Dr. Ploesser. But that doesn’t mean antidepressants can’t have their place in a healthy diabetes self-care plan.
“People living with depression and other mental health concerns have seen great success with the use of antidepressants, and it’s important that, if you’ve been prescribed a medication, you take that medication,” says Graham. “Just be sure to talk to your doctor about the possible side effects and to share any concerns with them as they come up.”
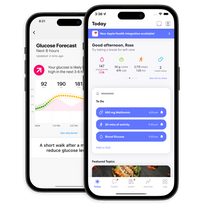
Along the way, your One Drop coach can also be there to support your decision-making process, answer questions between doctor appointments, and be your cheerleader when you need one.
This article has been clinically reviewed by Alexa Stelzer, RDN, LD, CDCES, clinical health coach at One Drop.