Read time: 12 minutes
- A1C has long been the gold standard for measuring diabetes management. But a new metric—time in range—is proving to benefit many.
- Time in range can provide a more comprehensive picture of glucose management and transform the way diabetes is managed.
- Through contextualization and storytelling, time in range offers people with diabetes an actionable narrative to optimize their diabetes experience.
If you’ve been diagnosed with diabetes, you are probably aware of the A1C test. Discovered in the 1960s, A1C was first suggested as a diagnostic tool for diabetes in the 1970s and became the gold standard in diabetes management metrics in 1993 when results from the Diabetes Control and Complications Trial (DCCT) proved that A1C level was the dominant predictor of diabetes-related complications.
To this day, A1C is used globally for both diagnosis and long-term monitoring of diabetes. The test allows providers to quickly approximate a person’s average blood sugar over the last three months. When blood sugar runs consistently high, those daily numbers will be reflected in a higher-than-normal A1C. The stark results from this test can quickly inform both patient and provider with insight into diabetes management protocols (or an actual diabetes diagnosis).
But as diabetes technology has evolved over the last two decades, so has the thought process behind using A1C as the sole metric to determine how diabetes is being managed. A1C fails to capture weekly, daily, and hourly diabetes data; it fails to contextualize the daily realities of living with diabetes. The wide range of blood sugar values associated with A1C is based on set averages, meaning that diabetes management based solely on A1C is an oversimplified application of a global population average to determine one’s health, which can be very misleading.
Results from an A1C test can lead to more questions than answers, leaving someone feeling more overwhelmed and defeated than motivated and empowered in their diabetes management.
Instead, those of us with diabetes should be looking to a new standard to measure our outcomes: time in range.
Time in range (TIR) is a tool that can help those of us living with diabetes better understand our daily outcomes (which, over time, lead to lifelong outcomes) and make swift adjustments to our diabetes regimen rather than waiting until our next A1C result.
Below, learn more about TIR and how using this metric, in conjunction with A1C, can bolster your diabetes management.
The Limits of A1C
TIR is the percentage of time that a person with diabetes spends with their blood sugar levels in a target range for optimal health outcomes. TIR goes beyond A1C in representing glucose levels because it captures the whole story: the highs, lows, and in-range values that characterize life with diabetes. It can be monitored regularly by the person living with diabetes and is far more actionable than a three-month averaged test. But why?
A1C is just an average. Two people could have the same A1C, but very different blood sugar realities on a day-to-day basis.
For example, someone may get the A1C they hoped for—their test result may meet their target goal. But what does the A1C truly represent? Perhaps it really does mean their blood sugar is at-target 99% of the time.
It can also mean high blood sugar half of the time and low blood sugar accounting for the other. As research continues to demonstrate, glucose variability (or fluctuations in blood sugar, as opposed to steady, consistent numbers) can be equally as detrimental as high blood sugar itself.
That one test result has all sorts of variations and meanings that don’t fully capture daily life with diabetes.

There’s also a mindset barrier that comes with A1C results.
That singular number can help or harm. It can help to validate a current regimen if you get the result you’d been hoping for. It can harm by leaving you feeling helpless, ashamed, and doomed for failure if you don’t reach that goal you had set for yourself.
When you have an idea of where you’d like your result to be but don’t get there, the A1C can become an elusive, seemingly insurmountable health target. It could be because of the way those of us in Western society attach ourselves to numbers and test results, a mindset we’re taught early on in school. But it could also be because that number—that we give so much authority to—tells us so little about our reality. On its own, an A1C gives us pretty limited insight into what’s happening every day.
Time in range, on the other hand, puts more context behind daily life with diabetes. It helps us to better see and understand our diabetes experience.
Defining Time in Range
Simply put, TIR is the amount of time a person with diabetes spends within their target blood sugar range.
That range varies person to person; it is a completely individualized target based on what you and your provider decide is best for you at a certain time. Someone newly diagnosed with diabetes may have a target of 100-180 mg/dL (5.6-10.0 mmol/L), while someone aiming for a more stringent goal may have a target between 70-120 mg/dL (3.9-6.7 mmol/L).
While some publications and organizations suggest a TIR target of 70-180 mg/dL (3.9-10.0 mmol/L), it should be noted that this is only a default range. TIR can and should be evaluated on a personal basis, based on various lifestyle factors. But, also important to note, if you are trying to achieve normal, non-diabetic blood sugar levels, it would be best to set a range that is lower than the average, suggested one.
The percent of time spent in your set range is also important when calculating TIR. Again, this is a very individualized metric that should be decided on with your provider. You may determine you want to set a very strict range (which could be more difficult to reach), while being more lenient with the time spent in that range, opting for a goal of 50% in-range. Conversely, you may set a blood sugar range for yourself that is broader, while making sure you fall within that range 90% of the time.
Once you decide on these two sets of targets—your blood sugar ranges and percent of time spent within that range—you will have your TIR goal.
Visualizing the Diabetes Experience
Perhaps the biggest benefit of using a TIR metric is the story it can tell those of us living with diabetes.
Unlike A1C, TIR is more subjective. It allows us to put a story to all of the numbers. Whether it’s data from continuous glucose monitoring (CGM) data or the numbers from a blood glucose monitor (BGM) screen, these data points are only that. They give us objective results, but it’s the story behind each number and data point that matters. When we can start to see a story unfold behind all of those unique data points, that is when we can begin to assess and adjust accordingly.
Without that story, though, the data is practically useless in helping us to make any sort of real change in our health goals. They only serve as a reactive measure.
One way to think about how this sort of narrative works is by considering data visualization. In the linked example, you can see the power of visually sorted data. Gathering massive amounts of data—whether from a CGM or BGM—is useless unless insight from that data is also generated.
Applying visuals or stories to our data, however, can bring those numbers to life; giving purpose and meaning to our data can help us turn it into a story, one that can help us better roadmap our diabetes experience.
But what does it mean to visualize our diabetes data?
If you have a CGM, this is something that can be done automatically using the manufacturer’s software. The results are rudimentary, showing (visually) the percent time spent in your target range using simplified, stacked graphs, color-coded by range. It allows for the user to quickly and easily ascertain where they are on their TIR spectrum.
Using BGM results, the process is a bit more manual, but still doable. The data sets you acquire will come from each fingerstick you take; the more times you can check your blood sugar, the more data you will have to apply to your story.
The process to manually calculate TIR is as follows:
[Blood sugar values that fall into your target range / total amount of blood sugars taken] x 100 =
amount of values in target range percentage
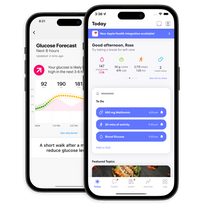
Using One Drop to See Your Time in Range
If you use the One Drop app, you can also see where your range falls visually. To get started, set up your blood sugar range in your App Settings, found under My Account. In Health Settings, slide the cursors in Blood Glucose Range to the targets you’d like to see.
Once you start tracking your blood sugar in your app (either using your One Drop meter, another blood glucose meter, or CGM data points), you’ll be able to see where your readings fall in your Insight tab. In the Last 7 Days screen, blood sugar readings will fall into the range that you’ve set, showing you the percent in-range in the middle, as well as the percentage of readings that fall below or above range on the left and right. Visually, these numbers are also represented by the magenta dots, falling either inside your target range (represented by the magenta bar in the middle) or outside. If you tap into your Last 7 Days screen, you’ll be able to see a further visual breakdown of your readings and where they fall on your spectrum.
The more often you check blood sugar and add it to your One Drop app, the more in depth your TIR visual results become. Think of it this way: you can’t manage what you don’t measure. Measuring your glucose will give you these visuals that you can study, learn from, and enact change to further optimize your diabetes plan.
While TIR is mostly only associated with a CGM experience, it can absolutely be used in combination with BGM management—the major caveat being that many blood sugar checks are needed in order to calculate a true TIR value.
You may have been told by your doctor that you only need to check your blood sugar once a day; perhaps you’ve been instructed to only check two hours after meals. To truly understand your time-in-range, you will need to check your blood sugar much more often than what is typically prescribed. In order to create and see patterns in our blood sugar data, we must have multiple blood sugars throughout the day: upon waking, right before eating breakfast, 20 minutes after breakfast, one hour after breakfast, and so on. We can’t see or know what we don’t measure, so it is imperative that many blood sugars are taken throughout the day in order for us to be able to draw any sort of accurate conclusions.
We realize checking blood sugar this often can be difficult for most to achieve due to insurers or discouragement from providers, which is exactly why we created an unlimited test strip offering. Many of us working at One Drop use this unlimited plan personally so that we can access a more complete and precise picture of our own diabetes management. Using standard metrics of care—like checking four times daily—leads to a large chasm of uncertainty and unknowing when it comes to not just TIR, but health outcomes overall.
Contextualizing the Diabetes Experience
Beyond visuals, there is the art of the story when it comes to diabetes. Each blood sugar reading is a reference point, usually a direct effect of some action.
Perhaps one of the most intriguing parts of the diabetes journey is just how rich it can be in narrative. Often, this part of diabetes is overlooked—when we are instructed to only look at blood sugar in a fasted state or limit ourselves to checking only three times a day, we miss out on our own story. Three data points of glucose in a given day amounts to nothing more than a sentence—thirty data points, however, can begin to shape a rich storyline.
This storyline can serve as a feedback loop for how we can enhance our unique diabetes experience. With an unlimited amount of variables—both external and internal—that we find ourselves up against daily, no one diabetes experience is the same. But when we take the time to gather these data points (blood sugar readings) and compare them to the TIR goals we set for ourselves, we begin to watch patterns unfold that tell us definitively what works, what doesn’t, and possibly even uncover new opportunities for us to try.
People can be told time and again that carbohydrates, sugar, and lack of exercise cause high blood sugar, but rarely does this information carry over to real-life change. A feedback loop, though, based on our own diabetes data can lead to increased awareness and subsequent behavior change. Observing that intuitive information playing out in our own reality can feel like an epiphany. Using TIR metrics helps us to better see and understand these narratives that play out daily in life with diabetes.
A1C, on the other hand, gives a quick, high-level overview of how someone is doing—it reads as a pass-fail, good-bad, black-white, right-wrong way of diabetes management that leaves no room for granularity or useful insight. Not to mention, this rigid mode of diabetes care can greatly impair mental health outcomes.
Think back to a time when you received a less-than-optimal A1C result. What did it do to your diabetes management? Did the result encourage you to do better, or leave you feeling defeated? Did your sub-par A1C empower you to really lean into your diabetes, or did it encourage you to neglect it?
While A1C results can (and should) be used to further enrich our diabetes story, we should be using them in tandem with TIR measurements that can facilitate more context around our detailed, daily narrative. A1C is still very much the desired metric for diabetes care, and that will not likely change anytime soon. But solely relying on A1C results can keep us stagnant in our health journey. Instead, we can optimize our health by supplementing A1C with TIR, a measure we can use on a daily or weekly basis to better understand our diabetes story. Using this mindset shift in the way we look at our blood sugar can mean greater outcomes in not just A1C results or average blood sugar, but overall health.
Choosing to lean into your diabetes story with TIR metrics can result in meaningful change for your future. Ultimately, it’s your data, your blood sugar—and it’s how you choose to use them that can make a significant impact on your health, and your life.
This article has been clinically reviewed by Lisa Graham, RN, CDCES, health coach and director of clinical operations at One Drop.