Read time: 5 minutes
- Blood glucose monitors (BGMs) require a finger-prick test and produce a single real-time reading; continuous glucose monitors (CGMs) use a subcutaneous sensor to automatically track blood glucose levels over time.
- Type 2 diabetes (T2D) accounts for 95% of all incidences of diabetes in the U.S., yet only ~3% of the T2D population use a CGM despite high levels of interest.
- Advancements in CGM technology, reimbursement policies, and digital health interventions to increase health knowledge and motivation may increase CGM access and help better meet the needs of millions living with type 2 diabetes.
Regularly checking your blood sugar, also known as self-monitoring of blood glucose (SMBG), is a critical component of diabetes management. A healthcare provider can use detailed information about glucose levels collected across time to assess your medications or insulin regimen. SMBG can also help inform adjustments you make to self-care behaviors, such as diet and exercise, to improve daily glycemic management.
What is the Difference Between a BGM vs. CGM?
While a blood glucose meter (BGM) requires a finger-prick test for each reading, a continuous glucose monitor (CGM) is a wearable technology consisting of a sensor placed just under your skin that automatically tracks glucose levels throughout the day and night. People living with diabetes rely on a BGM, CGM, or both to check their blood sugar. Unlike BGM, which only measures blood glucose at one moment in time, CGMs allow users to observe their glucose levels anytime at a glance, review changes over time, and see trends. It's not really a question of BGM vs. CGM as both can be critical in understanding your blood sugar and managing diabetes.

What Are the Benefits of Continuous Glucose Monitoring?
A CGM device can help make managing type 1 diabetes (T1D) or type 2 diabetes (T2D) easier. For example, continuous glucose monitoring can:
- Help paint a bigger picture: Because CGMs measure glucose levels every few minutes, the data generated can help you pinpoint the impact of certain foods, activities, and other lifestyle factors on blood sugar levels.
- Prompt personalized care: With guidance from a healthcare provider or One Drop clinical health coach, you can fine tune your care plan based on CGM data patterns and trends.
- Alert you to highs and lows: It’s common for CGM devices to beep or signal when glucose levels fall outside a safe range. Manufacturers designed this feature to give users enough time to take action before hypo- or hyperglycemia progresses.
- Limit finger-prick tests: While CGM users might still turn to a handheld blood glucose monitor to dose insulin or calibrate their device, overall, continuous glucose monitors significantly reduce finger-prick testing. Fewer finger pricks are often a salient point for people with type 1 diabetes or those who require more frequent BG checks.
CGM Attitudes and Adoption Among People with Type 2 Diabetes
Although continuous glucose monitoring can provide potentially life-saving benefits to people with diabetes, nationwide access to CGMs remains limited. Approximately 37.3 million people in the U.S. are living with diabetes (95% T2D; 35.4M), but only 6.4% (2.4M) use CGM, according to a 2021 market analysis by Seagrove Partners. While adoption rates are reasonable relative to the type 1 diabetes population, just over 3% of T2Ds use a CGM—that’s more than 34 million people with type 2 diabetes domestically without CGM access.
A false assumption is people with type 2 diabetes lack awareness of or interest in continuous glucose monitoring. New research from One Drop presented at the 82nd Scientific Sessions of the American Diabetes Association indicates otherwise. Ninety percent of T2D participants in a mixed-method study were familiar with continuous glucose monitoring, but 83% had never used a CGM. Still, they shared an overwhelmingly positive perception of CGM technology; most were open to adoption, valuing regular feedback, relief from blood glucose meter (BGM) fingersticks, convenience, and improved diabetes management.
"Trends that emerged in our research underscore a disconnect between public perception and demand and the accessibility of vital diabetes management technology," cautioned Dr. Lindsay Sears, SVP of evidence generation at One Drop. "While the benefits of continuous glucose monitoring for diabetes management are well understood, and interest continues to grow within the largest segment of the diabetes population (T2Ds), millions still lack access to CGM technologies. To understand why, we must look to the barriers put in place by device manufacturers, insurance providers, and government agencies."
Barriers to CGM Access
Unfortunately, interest in continuous glucose monitoring is not enough to ensure someone with diabetes has access to a CGM device. Below are well-known barriers limiting widespread adoption.
- High costs: Producing and marketing an FDA-approved continuous glucose monitor comes at a high price. Today, associated costs trickle down to private insurance companies and government systems who want to see savings within three years or the end-users who can end up paying up to $500 out-of-pocket per month for a CGM.
- Insurance limitations: While anyone can purchase a blood glucose meter, prior authorization is required for coverage of continuous glucose monitoring devices to determine medical necessity. Most T2Ds do not meet a strict set of criteria, including managing your diabetes with insulin.
- Health inequities: In the United States, historically marginalized communities have lower access to quality care and higher rates of illness, including diabetes-related health complications, but discrepant access to vital diabetes management technology like CGMs.
- Cognitive burden: More is not always better. Continuous access to blood glucose data can become overwhelming without context from other health information (e.g., carb intake, physical activity) or guidance on what to do next.
- Dermatological concerns: Traditional CGMs require inserting a needle into the fatty tissue just below the skin, typically on the upper arm or stomach, which may cause pain or discomfort. Hypersensitivity reactions, contact dermatitis, and scarring are among the most commonly reported problems caused by diabetes device adhesives.
The Next Generation of CGM
Seagrove Partners estimates that T1D CGM penetration jumped by more than 30% between 2018 and 2021, suggesting future growth opportunities will primarily stem from the T2D segments. However, success hinges on advancements in device technology, reimbursement policy, and digital health interventions to increase health knowledge and motivation are warranted to better meet the needs and preferences of millions currently living with type 2 diabetes.
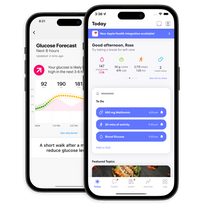
One Drop plans to enter the continuous health sensing market with a daily disposable, minimally invasive biosensor in development designed to provide greater flexibility and insights for people living with diabetes compared to blood glucose monitor (BGM) fingersticks alone. The availability of our continuous health sensor is subject to receipt of clearance or approval from the U.S. Food and Drug Administration. Pending regulatory approval and commercial adoption, we believe integrating the One Drop health sensor with our existing digital solution, One Drop Premium, should augment proven outcomes and yearly cost savings for members living with diabetes and other chronic conditions.
This article has been clinically reviewed by Lisa Graham, RN, CDCES, clinical health coach and director of clinical operations at One Drop.