Recognizing the first signs of diabetes can be difficult for multiple reasons. Not only can they come on subtly and gradually—making it hard to notice anything is amiss in the first place—but accepting the chronic experience of living with diabetes can be mentally and emotionally challenging as well. As with any health issue, though, knowledge is power. Read on to learn more about the first signs of diabetes and what you can do to address them.
Common First Signs of Diabetes
First, let’s remind ourselves what diabetes is, exactly: a chronic health condition that affects the way your body metabolizes glucose (a.k.a. sugar) and converts food into energy.
While the causes of type 1 and type 2 diabetes are different—the former being an autoimmune condition that leads to the death of beta cells in the pancreas, which make insulin (a hormone that regulates your blood sugar), and the latter being a more lifestyle-related condition that leads to long-term beta-cell dysfunction, rather than death—the symptoms are relatively similar.
Per the American Diabetes Association (ADA), common first signs of type 1 and type 2 diabetes include:
- Frequent urination (polyuria)
- Excessive thirst (polydipsia)
- Excessive hunger, even though you're eating (polyphagia)
- Extreme fatigue
- Blurry vision
- Cuts/bruises that are slow to heal
- Weight loss, even though you're eating more (type 1)
- Tingling, pain, or numbness in the hands/feet (type 2)
But what are the underlying processes happening in the body that connect these symptoms to diabetes?
It’s all about understanding basic glucose metabolism, says One Drop coach, Lisa Goldoor, a registered nurse (RN) and certified diabetes care and education specialist (CDCES). “We eat carbs, which are broken down in our gut and absorbed into the bloodstream,” she explains. “The pancreas is then signaled to release insulin, which is what helps the sugar get into the cells, where they’re used for fuel.”
When insulin is “missing” from that equation, continues Goldoor—whether it’s because your body isn’t producing enough or resisting it—glucose builds up in the bloodstream. “Your body is smart enough to recognize this and to try to get rid of that extra sugar by peeing it out,” she explains. “That’s why frequent urination (polyuria) is a common symptom of diabetes. And, with extra urination, the body signals to the brain that you’re dehydrated, so excessive thirst (polydipsia) is also a symptom.”
Meanwhile, as glucose remains stuck in the bloodstream, your body’s cells crave the fuel and energy they’re not getting, “so those cells signal to the brain that they’re hungry, which causes excessive hunger (polyphagia),” explains Goldoor.
These are the most common symptoms, she adds, but you can also experience lethargy and fatigue (due to lack of energy when cells don’t get enough glucose), nausea and vomiting (a possible result of swelling and inflammation in the pancreas if diabetes is unmanaged), and frequent UTIs (due to excessive sugar in the urine, which can promote bacteria growth).
As for blurry vision, slow healing, and numbness or tingling in the hands and feet, these symptoms are “more related to complications of chronic high blood sugar,” notes Goldoor. “The blood itself gets ‘thicker’ with the extra glucose (glucose attaches itself to our red blood cells), which makes it harder for our blood to travel to all the tiny blood vessels in the body, especially the eyes and feet. That impaired circulation also affects healing, as we need extra blood flow to injured areas.”
Comparing and Contrasting the First Signs of Different Types of Diabetes
Again, most of the first signs of diabetes (regardless of the type) are the same—but not all of them.
Weight loss, for instance, is a common first sign of type 1 diabetes because, once glucose is stuck in the bloodstream, the body begins to burn fat for fuel instead, explains Goldoor. Even though glucose isn’t absorbed properly in type 2 diabetes either, these initial symptoms come on much more suddenly in type 1 diabetes, as the lack of insulin associated with the condition can be fatal, so your body reacts as quickly as possible to keep you alive, she says.
But in type 2 diabetes, your cells still make some amount of insulin; your body just doesn’t respond effectively to it (a condition known as insulin resistance). As a result, your body gradually tries to produce more insulin over time in an attempt to counteract insulin resistance, which signals the muscles and liver to store blood sugar. However, once their storage is full, your liver sends the extra blood sugar to fat cells to be stored as body fat, which can lead to weight gain. That’s why it’s common for people to experience type 2 diabetes and obesity simultaneously, notes Carrie Lam, MD, co-founder and medical director of Lam Clinic in Tustin, California.
Plus, adds Dr. Lam, “high insulin levels prohibit the release of serotonin, a neurotransmitter in the brain that informs the body to slow down eating. Without serotonin, there’s a tendency to overeat, which then leads to a spiral of excessive sugar intake,” raising the risk of insulin resistance and, in turn, type 2 diabetes. “As diabetes sets in,” explains Dr. Lam, “so can lethargy and inactivity, contributing further to the vicious cycle of weight gain and worsening of diabetes.”
With the gradual nature of type 2 diabetes in mind, “routine doctor visits and bloodwork panels are your best tools to recognize prediabetes and type 2 diabetes,” as well as gestational diabetes, continues Goldoor. “Gestational diabetes happens when the pancreas can’t keep up with the extra demand for insulin since the placenta makes extra glucose for the baby,” she explains. “This is usually picked up between 24 and 28 weeks of pregnancy with an oral glucose tolerance test, so the best way to diagnose gestational diabetes is through routine prenatal care.”
Next Steps After Noticing the First Signs of Diabetes
Now that you know a little more about the first signs of diabetes, what will your first steps be if or when you begin to notice those symptoms?
One Drop coach, Hanna, a CDCES and registered dietitian/nutritionist (RDN), recommends going to your primary care doctor first and asking for an A1C lab test, a simple blood test that measures your average blood sugar levels over the last three months.
“If your A1C test result is 6.5 or above, then a diagnosis of diabetes is given, and the care plan begins,” explains Hanna, who notes that the A1C test alone does not distinguish different types of diabetes. “Because type 2 diabetes is a lot more common overall, and especially in adults, it is often assumed that the person has type 2 diabetes,” she says. “But you can always ask your doctor what they think.”
From there, continues Hanna, you might choose to get a referral to an endocrinologist or stay with your primary care doctor. “Many primary care doctors can manage type 2 diabetes well, so needing an endocrinologist will depend on your circumstances (your primary care doctor, the severity of your diabetes, your preference, type 1 vs. type 2, etc.),” adds Goldoor.
If you’re diagnosed with type 1 diabetes—meaning your pancreas doesn’t produce insulin at all—your doctor will teach you how to monitor your blood sugar on your own and administer multiple daily insulin injections with a pen, syringe, or pump. They’ll also help you figure out nutrition- and exercise-related habits that work for your lifestyle and health condition.
If you’re diagnosed with prediabetes, type 2 diabetes, or gestational diabetes, your doctor may recommend medication in some cases, or that you monitor your blood sugar at home with a glucose meter kit. Regardless of your circumstances, they’ll almost certainly recommend a few lifestyle changes (think: more exercise, fewer refined carbs, less saturated fat, and more healthy fats and fiber).
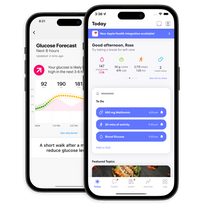
“Referral to a dietitian/nutritionist or certified diabetes care and education specialist can help determine which foods are best for you,” says Carmen Echols, MD, a board-certified family medicine physician based in Atlanta, Georgia. “There are still a variety of foods that may appeal to your palate that you can incorporate as part of your new lifestyle change.” (One Drop health coaches include registered dietitians/nutritionists, certified diabetes care and education specialists, registered nurses, and other qualified health professionals who can help you manage diabetes.)
No matter who’s on your care team, “know that there is a lot of support out there and that you are not alone,” adds Hanna. You might experience a range of emotions at first, says Goldoor, and that’s okay. “It’s about getting to a place of acceptance and knowing it’s not a linear journey for everyone.”
Think of it as an opportunity to take stock of your health, continues Goldoor. Where can you make improvements? What are your goals? What are your barriers? Where can you fit in time to devote to your health on a daily, weekly, or monthly basis? What does that look like for you?
As Dr. Echols says: “Diabetes may be life-changing, but it’s not life-ending.”
This article has been clinically reviewed by Jamillah Hoy-Rosas, MPH, RDN, CDCES, and VP of clinical operations and program design at One Drop.