Para español, haz clic aquí.
Every year, between 2% and 20% of all pregnancies in the U.S. are affected by gestational diabetes, according to the Centers for Disease Control and Prevention (CDC). Before learning how to treat gestational diabetes, it’s important to understand what the condition is and how it develops.
Gestational diabetes (or GDM) is a type of diabetes that is diagnosed during pregnancy—a time when your body goes through a lot of hormonal changes, some of which cause insulin resistance, meaning your body isn’t able to use insulin effectively. All pregnant people have some insulin resistance during late pregnancy (starting around approximately 24 weeks), but if the pancreas cannot make enough insulin to compensate for the level of insulin resistance, elevated blood sugars can develop. Gestational diabetes is diagnosed when blood sugars exceed certain targets (such as a blood sugar level of 190 mg/dL, or 10.6 mmol/L).
In some cases, it’s possible to have had insulin resistance before pregnancy without realizing it. But preexisting insulin resistance is just one among many possible risk factors for gestational diabetes.
Understanding Gestational Diabetes Risk Factors
According to the CDC, other factors that can increase the risk of developing gestational diabetes include:
- Being older than 25
- Entering pregnancy at a higher weight and/or not being physically active
- Family history of type 2 diabetes
- Being a member of some ethnic groups, such as Hispanic/Latino, Black/African American, American Indian, and Asian American
- History of gestational diabetes in a previous pregnancy
- Having previously delivered a baby weighing more than nine pounds (four kilograms)
- Having polycystic ovary syndrome (or PCOS, which can cause insulin resistance) or prediabetes
- High blood pressure (greater than 140/90 mmHg) or heart disease
Typically GDM doesn’t have any symptoms, so if you have any concerning risk factors, your doctor may recommend testing your blood sugar levels at your first prenatal visit. For most people, though, regardless of risk factors, blood sugar testing will be performed at weeks 24 to 28 of pregnancy.
If GDM is identified, the next step is to develop a plan with your doctor on how to treat gestational diabetes and ensure that you and your baby stay healthy. When blood sugars stay elevated and unmanaged during pregnancy, the parent has an increased risk for cesarean section, preeclampsia (high blood pressure during pregnancy), and, after pregnancy, type 2 diabetes. Meanwhile, the baby can also be at risk of macrosomia (larger-than-average baby), premature birth, complications at birth, low blood sugar at birth, and, later in life, type 2 diabetes.
How to Treat Gestational Diabetes
The good news is that you can successfully manage gestational diabetes and reduce the risk of complications by following your GDM care plan.
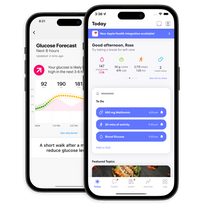
While that plan may look slightly different from person to person, generally speaking, you’ll want to focus on healthy eating, exercise, monitoring your blood sugars multiple times a day, managing stress, attending appointments with your medical team, and, if necessary, taking medication. (Having access to blood sugar predictions and insights can be a gamechanger, too.)
Food Matters
Think of what you put into your body like gusts of wind to your blood sugars. Certain foods will have a stronger force and elevate your blood sugar, whereas others may raise it slightly or not all. Food can be categorized as mostly fats, carbohydrates, or protein.
Carbohydrates (a.k.a carbs) cause blood sugar to rise. They break down into sugar (glucose) that enters the bloodstream, where they can be used as energy. With GDM, however, your body can’t efficiently move sugar from the blood into the cells for energy. For this reason, carb-heavy foods can cause elevated blood sugars.
But that doesn’t mean you have to avoid carbs altogether. Carbohydrates can still play a role in nourishing you and your baby. Learning how to follow a healthful eating pattern and choose the right types and right amounts of carbohydrates can help you maintain healthy blood sugar levels.
Keep your meals on a schedule and distribute your carbs. The current recommendations on meal planning for gestational diabetes are to eat small, frequent meals. Three meals and three small snacks are usually recommended to distribute your carbs throughout the day and get the calories you need to support a healthy pregnancy and the growth of your baby. Whereas large meals may increase the risk of elevating your blood sugar, small meals staggered across a consistent schedule ensure you’re not consuming too many carbs at once and spiking your blood sugar.
Make the right food combination on your plate. Combine lean protein, plant-based fats, and non-starchy vegetables with your carbs to slow digestion and reduce the risk of spikes in blood sugar. Start by filling half of your plate with non-starchy vegetables such as broccoli, asparagus, cauliflower, spinach, or leafy greens. Divide the other half in two, and fill one-fourth of your plate with protein-rich foods, such as fish, chicken, or lean meat. Complete your plate by adding high-fiber sources of carbs, such as sweet potato, beans, brown rice, quinoa, or buckwheat. To incorporate healthy fats, try using avocado oil for cooking or olive oil in a salad dressing.
Eat healthy without compromising flavor. Healthy eating isn’t just about nutrition and portion sizes; it’s also about enjoying foods that you genuinely love—whether because they’re simply comforting or because they’re an important part of your culture and traditions. Either way, celebrate your food with herbs and spices that enhance the flavor in your meals and help you reduce the amount of salt. Add fresh cilantro, tarragon, or chives to your salads and vegetable soups. Sprinkle some cayenne pepper and squeeze citrus fruits such as lemon or lime on your fruits and vegetables.
Remind yourself that you’re in control. Take a pause before reaching for food and ask yourself: “Am I actually hungry?” If the answer is “no,” emotions may be driving the urge to eat. At this point, finding a different way to cope with those emotions—such as going for a walk, taking a deep breath, drinking water, or calling a friend—could be helpful. Plus, did you know that we can easily mistake thirst for hunger? Next time, drink some water and wait to see if you feel better.
If it turns out that you are hungry, make a healthy choice your first choice. Here are some healthy swaps to consider during your next craving.

Exercise and Blood Sugar
Exercise can help with managing your blood sugar because it makes your body more sensitive to insulin and may reduce insulin resistance.
For pregnant people, the American College of Obstetrics and Gynecologists (ACOG) recommends 150 minutes of moderate-intensity aerobic activity (think: brisk walking, gardening) per week, split into whatever way works best for you. For some, that might mean five 30-minute workouts each week, while others might find it more realistic to squeeze in a few 10-minute sessions each day when they can.
Either way, if you’re new to exercise or want to try a new activity, be sure to talk to your doctor first, as those who take insulin or other oral medications to lower blood sugar may be at risk for low blood sugars during or after exercise.
As for when you work out, exercise is great at any time of the day, but it may be especially helpful immediately following a meal. According to a study published in the journal, Frontiers in Endocrinology, glucose levels tend to peak within 90 minutes of a meal. Consider engaging in physical activity, such as a 15 to 20 minute brisk walk, after a meal to reduce post-meal blood sugar levels.
Find it challenging to get started or stay motivated? Try the following exercise tips:
Start small. Sometimes we set the bar so high for ourselves that we can’t even reach it. Fortunately, studies have shown that even five to 10 minutes of exercise at a time, if done consistently, can add up to big results. So, if a 30-minute routine feels too daunting, start with 10-minute increments throughout the day. Here are some examples of activities you can include in a 10-minute exercise routine:
- Walking
- Dancing in your living room
- Cleaning your home
- Doing some light yard work
- Standing up and moving during a TV show
Find a buddy. Let your neighbors or a friend know about your exercise goals and invite them to work out with you. Having someone to exercise with can make it more fun and keep you motivated. That said, working out with others may be challenging during COVID-19; to stay safe, consider going for a walk with a friend and wearing a face mask during your stroll.
Keep it fresh. Anything we do over and over every day can get boring at some point, no matter how motivated we are. Find several activities you enjoy or would like to try. When you get bored with one, switch it up! You could try a dance class for some days and then switch to yoga. (Or, try these no-equipment exercises for a quick total-body workout.)
Reward yourself. Rewards can help motivate you to achieve your exercise goals. Try offering a small reward to yourself if you reach your goal for the week—for instance, if you met your goal of walking four days this week, treat yourself with a new pair of walking shoes or workout clothes. (Here are more creative ways to reward yourself the next time you reach your goals.)
What Comes After Your Baby is Born
You may be wondering what happens with gestational diabetes after you’ve delivered your baby. In most cases, your blood sugar returns to normal after giving birth. However, having gestational diabetes puts you at a higher risk of developing type 2 diabetes in the future.
The only way to know if you still have diabetes after pregnancy is by testing your blood sugar levels. That’s why it is very important that you return to your OB-GYN for your postpartum visit. Your first postpartum visit will likely be around four to 12 weeks after delivery, at which time your doctor will use a blood test to determine if you still have diabetes.
Approximately 60% of women with gestational diabetes will go on to develop type 2 diabetes in their lifetime. Focusing on the below lifestyle factors can help you delay or prevent the development of type 2 diabetes in the future:
- For those who are classified as overweight, research shows that you can reduce the chances of developing type 2 diabetes by losing 5% to 7% of your weight and keeping it off. (Reminder: Weight loss plateaus are totally normal—here’s how to navigate them.)
- Engaging in at least 30 minutes of physical activity five days a week can reduce insulin resistance and help promote weight loss.
- Follow a healthful eating pattern and stay mindful of portion sizes and food choices.
- Consider asking your doctor to refer you to a diabetes prevention program, or working with a One Drop coach who specializes in diabetes prevention.
Reducing Your Risk of Gestational Diabetes for Future Pregnancies
Even if your blood sugars return to a healthy range after giving birth, you’re still at an increased risk of developing GDM in subsequent pregnancies. You can reduce your risk by achieving a healthy weight, following a nutritious diet, and staying active. Know that by taking good care of yourself, you’re also taking good care of your children.
Whether you’re ready to create your own GDM treatment plan or you simply want to make sure your blood sugar levels stay in a healthy place, become a One Drop Premium member and explore our Complete Diabetes package to find the best approach for your lifestyle.
This article has been clinically reviewed by Jamillah Hoy-Rosas, MPH, RDN, CDCES, and VP of clinical operations and program design at One Drop.