You've almost certainly heard of heat stroke, but if you live with a heart condition such as high blood pressure, it's especially important to know how to distinguish heat stroke from other potentially less serious heat-related conditions, such as heat cramps and heat exhaustion.
Summer may be on its way out, but temperatures often continue to climb throughout August and even the early fall months. So, even though you might already be gearing up for the change in seasons, the risk of heat stroke can remain very real—especially if you live with a chronic heart condition.
How Heat Affects Your Heart
When you’re exposed to heat and warm temperatures, your body—in particular, your heart—works hard to cool you down.
“In hot weather, core temperatures rise, and heat must be released from the body,” says Sadi Raza, MD, a board-certified cardiologist based in Dallas, Texas. Your body does this by increasing blood flow to the skin via a process called vasodilation (or opening of the blood vessels), he explains.
To maintain healthy blood pressure levels in the presence of vasodilation, continues Dr. Raza, your cardiac output (the amount of blood pumped by your heart per minute) must also increase. “This adaptive mechanism often manifests in us sweating more, which is the natural response to overheating,” he adds.
Most healthy people tolerate these changes without missing a beat (pun intended). But those who live with a heart condition may be more vulnerable to heat stroke, says Lutz Petersdorf, MD, vice president, Bayer Head of Global Medical Category Allergy & Cough/Cold, Pain & Cardio.
“Damage from a heart attack can keep the heart from pumping enough blood to get rid of heat,” which leaves you feeling overheated, he explains. “Cholesterol-narrowed arteries can limit blood flow to the skin as well.”
Plus, he adds, the combination of dehydration and increased blood flow to the skin may cause blood pressure to drop so low that it leads to dizziness or falls.
So, what can those with heart health issues do to make sure they’re staying safe in the heat? Here are some basic tips to follow.
Be Mindful of Heart Health Medications
When you’re sweating in hot weather, you’re removing water and salt from your body, explains Dr. Raza. So, if you happen to be taking any medications that do the same—such as diuretics (water pills), a common treatment for high blood pressure—you could run into some trouble with how much water your body is losing.
“For those on diuretics, insensible water loss from excessive sweating can lead to kidney failure,” says Dr. Raza. “In addition, medications such as beta blockers can prevent the body from increasing its heart rate as a natural response to heat.”
Other heart medications that can affect the body’s response to heat include ACE inhibitors (which widen the blood vessels to lower blood pressure), calcium channel blockers (which lower blood pressure and slow your heart rate by preventing calcium from entering the cells of your heart and arteries), and low-dose aspirin (used for heart attack and stroke prevention), notes Dr. Petersdorf.
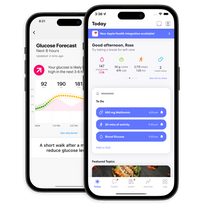
Despite these potential risks, says Dr. Petersdorf, no one should start or stop any medication without consulting their doctor. (And, if keeping track of your medications ever gets confusing, you can always use the One Drop app to stay organized.)
Be Strategic with Any Outdoor Activities
The sun is always highest (and feels the hottest) between about 12 and 3 p.m. So, when temperatures are climbing, your best bet is to limit outdoor activities during those hours to avoid any risk of overheating.
When you are outside, try to take it easy with whatever activity you’re doing, especially if you’re working out. “Reduce your exercise pace on hot days with high humidity,” suggests Dr. Petersdorf. “If the temperature is above 80 degrees Fahrenheit and humidity is above 80%, it’s best to postpone your activity until it cools off.”
For any workouts longer than 30 minutes, Dr. Petersdorf recommends drinking eight to 12 ounces of water 20 to 30 minutes before exercising, plus six to 12 ounces more for every 30 minutes of exercise, to prevent dehydration.
You can also find more creative ways to stay hydrated: Whip up a batch of sugar-free DIY fruit popsicles or a smoothie packed with refreshing fruits like berries and bananas, suggests One Drop coach, Lisa Graham, a registered nurse (RN/BSN) and certified diabetes care and education specialist (CDCES). Another option is to fix yourself a crudité platter of water-rich produce like melons, grapes, cucumbers, celery, and lettuce. (Remember to check your blood sugar before and after trying new foods to understand how they impact your health. And, if you have questions, your One Drop coach is just a text away.)
Regardless of how you hydrate, remember to wear lightweight, breathable clothing when venturing outside, such as loose-fitting cotton T-shirts, shorts, and, for extra caution, a brimmed hat.
Know the Symptoms of Heat Stroke
First, know that heat stroke is different from heat cramps and heat exhaustion. Heat cramps (considered the “mildest” heat-related syndrome) are involuntary, painful muscle spasms that usually happen as a result of fluid and electrolyte loss from heavy exercise in hot environments. The spasms, which typically happen in the calves, arms, stomach, and back, can usually be resolved by simply resting, cooling down, hydrating, and gently stretching or massaging the affected muscles.
Heat exhaustion symptoms, on the other hand, can include not only muscle cramps, but also faintness, dizziness, heavy sweating, rapid pulse, low blood pressure upon standing, nausea, and headache.
And, if left unaddressed, heat exhaustion can quickly lead to heat stroke, which can be much more dangerous.
“With heat exhaustion and heat stroke, many of the symptoms are similar,” explains Graham. But heat stroke can be life-threatening because, in those circumstances, your body temperature rises above 104 degrees Fahrenheit. Regardless, she says, it’s important to act quickly in both situations because, either way, your body is essentially incapable of cooling itself down without assistance.
Keep in mind that heat stroke symptoms may be even tougher to spot for those who live with diabetes or high blood pressure, adds Graham. “Heat stroke can mirror some of the symptoms that those with diabetes and high blood pressure may feel when their numbers are higher, such as dizziness, confusion, nausea, and vomiting,” she explains.
In the event of heat stroke, you’ll want to call 911 ASAP, says Graham. “While waiting for help to arrive, you want to get the person out of the sun, fan them, and use cooling measures like cool towels to try and help bring down their body temperature.”
If you're looking to monitor your blood pressure, check out the One Drop Complete Blood Pressure package or learn more about how our health coaches can help you achieve Complete Health.
This article has been clinically reviewed by Jamillah Hoy-Rosas, MPH, RDN, CDCES, and VP of clinical operations at One Drop.