On the hunt for the most accurate blood glucose meter? This post is for you.
Below, we put 10 of the best blood glucose meters on the market to the test to find which is the most accurate blood glucose meter.
Are Blood Glucose Meters Accurate?
First things first: Let’s talk about accuracy and blood glucose meters.
A few months ago, I read a post on blood glucose meter (in)accuracy that was quite alarming. Chris Hannemann, who has type 1 diabetes and is an OpenAPS'er, tested five of the best blood glucose meters for accuracy and found major discrepancies.
The overall variability between the meters studied by Hannemann was roughly ±11%, and two of the meters—both from the same manufacturer—showed major bias.
Hannemann had been using one of those meters to calibrate his continuous glucose monitor (CGM) and consistently found that his lab-measured A1C would come in a full percentage point higher than his CGM average would predict. For example, the meter-calibrated CGM data would correspond to an A1C of 6%, but laboratory-measured A1C would actually be 7%.
As someone who wears a CGM and always strives to achieve an A1C of 6.0% or lower, this post freaked me out.
Before I go on, I should mention your average blood glucose on your meter might not always correspond with your A1C results — and that doesn't necessarily mean your meter is bad!
Nevertheless, if I'm calibrating my CGM with a meter whose results are always off by that much,how can I be sure about reaching my targets?! I was also skeptical when I saw Chris' post because my A1C has always matched my predictions (based on my CGM average).
So, I decided to run my own test on the 10 best glucose meters from various manufacturers. Below I describe the test and discuss the results.
I should mention my favorite blood glucose meter is available here.
The Test
The Meters We Tested:
- Accu-Chek Aviva Connect
- Contour Next EZ
- OmniPod PDM FreeStyle Meter
- FreeStyle Lite
- Livongo InTouch
- OneTouch Ultra Mini
- One Touch Ultra 2
- Walgreens True Metrix Air
- Walgreens True 2 Go
- Wal-Mart ReliOn Confirm
These 10 meters varied in age and wear. Some were old, some were new;one was my own personal meter that I used to calibrate my CGM and make mission-critical decisions each day.
All of them passed their respective control solution tests, so it's safe to assume that they were in good working order. I tried to match the testing method employed by Chris (author of the original post) as closely as possible.
The Procedure
Eight rounds of testing were performed over the course of 24 hours according to the following procedure:
- Wash and dry hands
- Arrange meters on table in random order
- Insert new lancet into lancing device
- Remove test strip from each meter’s strip vial and insert strips into meters
- Wipe fingertip with alcohol pad and wait for it to dry
- Prick fingertip and squeeze out large drop of blood
- Apply blood to each test strip in order
- Record results
Notes:
- Order of meters was randomized for each round
- Tests were performed only when CGM readings were stable (i.e. no insulin on board and CGM showing a slope of 0 mg/dL/min)
- I didn't do anything special to stabilize my blood glucose—just tested as I went about a normal day
- The test strips used for each meter all came from their own unique vials
- Before and after completing the eight testing rounds, the meters were checked using their respective control solutions; They all passed the control solution tests
The Results
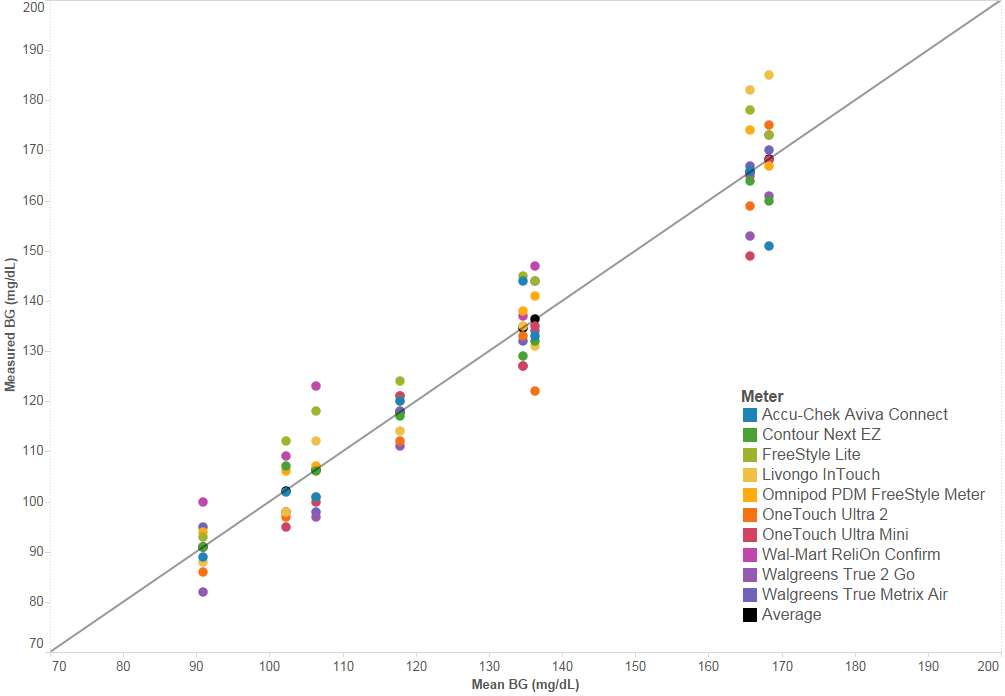
BG Results For Each Round, Compared:
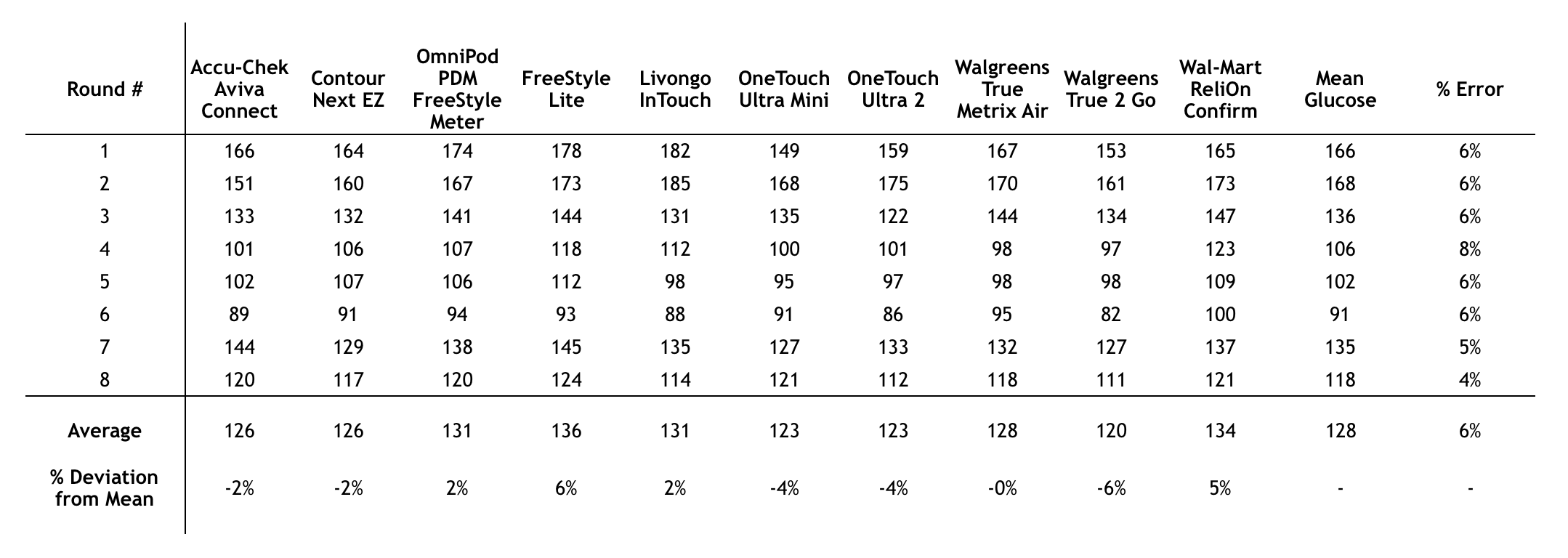
Unlike Chris, I didn't have an alarming spread in my results for any round. The overall between-meter variability ("% Error", or "%CV" for you stats folks) was only 6%.
In plain English: My treatment decisions wouldn't have varied much at all, regardless of the meter I was using.
One unit of rapid-acting insulin brings my blood glucose down by 80 mg/dL, and I correct it whenever I'm over 100 mg/dL. I'll usually correct down to 70-110 mg/dL, depending on my plans for the next couple hours (e.g. a big meal = correct to 70; workout = correct to 110).
I was relieved to see that even if I took a correction bolus for the maximum blood glucose of each round, I still would have been brought down to a desirable blood glucose level.
For example, take round 1 of testing. The highest reading I saw was 182 md/dL, and I'd take 1 unit for that. Even if we assume the true glucose was the lowest value from that round, 149 mg/dL, I'm still in good shape taking 1 unit because I'd only go down to 70 mg/dL.
What Does this Mean for A1C?
To figure out what this means for A1C estimates, let's take a look at how each meter's average value over the 24 hours of testing compares with the overall average across the entire list of these best blood glucose meters.
(NOTE: I realize that the average across this list of the most accurate blood glucose meters may not represent true A1C, but this comparison is useful to show that, no matter what meter you use, you're getting roughly the same results for averages and, thus, roughly the same estimated A1C.)
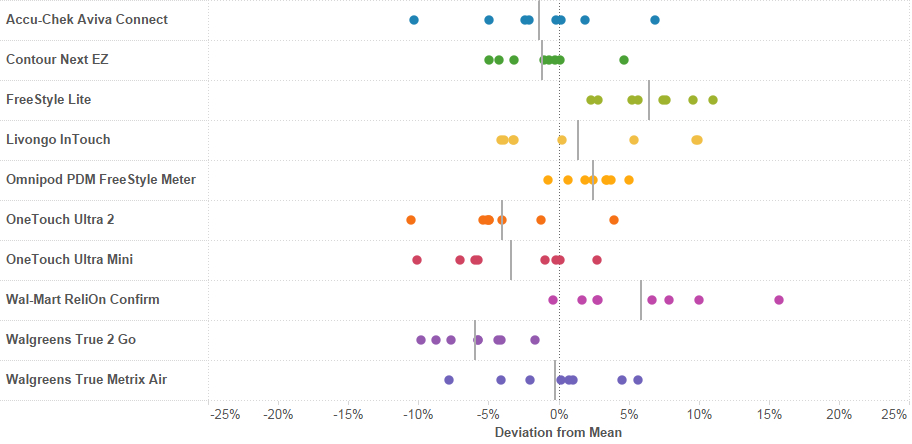
Looking below at the deviation from the mean—i.e, how much each meter's average value (solid gray line) differed from the overall average value (dotted gray line down the center)— I like what I see!
The average blood glucose from this list of the best blood glucose meters on the market(solid gray line) was pretty close to the overall average (dotted line down the center), with the greatest deviation at around 6% (FreeStyle Lite & Walgreens True 2 Go).
(Compare Chris' results, where max deviation was 14%.)
This means an estimated A1C calculated based on the average value from any of these meters would be roughly the same.
For example: If your average blood glucose on your meter was 154 mg/dL, that would translate to an estimated A1C of 7.0%.
- If you arrived at that average using a Walgreens True 2 Go, which appears to consistently report lower values, your actual A1C might be closer to 7.3%.*
- If you arrived at that result using a FreeStyle Lite, which appears to consistently report higher values, you may be pleasantly surprised by an actual A1C of 6.7%.*
I think most of us would agree that this is an acceptable degree of variation between estimated and actual A1Cs.
* Important note: This is just based on the data I collected for the specific meters I had in my possession. I can't say whether these trends would be true for all meters of any particular brand that I tested.
My Own Experience With Self-Measured Blood Glucose Averages and A1C
My CGM averages have always been correct when it comes to predicting A1C. Last summer and fall, I was using the Omnipod PDM FreeStyle meter (same one tested here) to measure my blood glucose values and calibrate my Dexcom CGM.
For September, my Dexcom showed a 30-day average of 132 mg/dl, which correlates to an A1C of 6.2%. That's exactly what my lab-measured A1C was in September.
For the past three months, I've been on MDI and using a Freestyle Lite to calibrate my CGM. Right before my latest A1C (1 week ago), Dexcom's 30-day average showed 117 mg/dl, which correlates to an A1C of 5.7%. My lab-measured A1C was 5.8%.
This is pretty much how it's always been for me. Not the A1Cs— I wish!—but the match between estimates and actual results. I've never had any reason not to trust my blood glucose meter readings because the results always lined up.
I do want to take some time to explain that even if the numbers don't line up, it doesn't necessarily mean your meter is to blame or that you haven't found most accurate blood glucose meter.
What about the post that started all this? Why were those results so off?

The truth is: I don't know. I actually own the meter that Chris uses — OneTouch UltraLink — and have used it for 4 years back when I was on a Minimed pump.
Unfortunately, I didn't have it with me at the time of this experiment, but I've tested with it a bit recently and the results are generally within 10 mg/dL of my FreeStyle Lite readings!
I'm not sure why Chris' results were so different. He's been using his OneTouch UltraLink for about 7 years, whereas mine only got about 4 years of use before being carefully stored at my parents place with all my other diabetes testers, a.k.a "antiques." I wouldn't be surprised if after a significant amount of wear, these things just don't work as well.
However, that doesn't explain why some of the other meters also deviated significantly from the mean glucose value.
It may be the test strips...
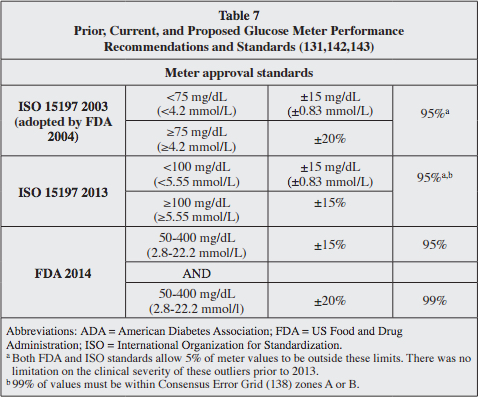
GM Consensus Statement, Endocr Pract. 2016;22 (No. 2)
The FDA requires that all new meters meet particular standards (shown above in Table 7), but once a meter is approved, the FDA does nothing to monitor accuracy. This is significant because although the meters may have functioned perfectly when approved by the FDA, that was with a particular set of test strips.
Test strips can vary from batch to batch
Test strips contain an enzyme that converts glucose into an electrical current that runs through the test strip and is displayed on your meter as a glucose concentration. Put simply: this is a blood glucose reading.
Since enzymes are proteins, they can break down due to humidity, temperature, and many other factors. So, differences in the environment where the test strips are manufactured, stored, and used can lead to differences in the blood glucose measurements they provide.
Those differences may be OK— the blood glucose values provided by these strips may still fall within the FDA's standards— but when comparing one batch of strips to another, things can get hairy.
For example, suppose one batch of test strips yields blood glucose readings that are 10% too high, while another batch (for a different meter, by a different manufacturer, or even for the same meter by the same manufacturer) yields readings 10% too low.
Even though each of these batches of strips might have an acceptable difference from the true blood glucose value, there is a 20% discrepancy (bias) between them. The differences could be clinically significant, especially when combined with a 7% random error on top of the 10% systemic bias.
So, where does this leave us?
More testing should be done! I feel pretty good about meter accuracy based on my own experiment and personal experience, but I'd feel even better if more people conducted similar experiments and got similar results about the most accurate blood glucose meters on the market.
Results like Chris' are scary—they make us feel like no matter how hard we try, we may still be missing the mark. The consequences go beyond the emotional toll, too. Meter and test strip inaccuracy may lead to results that fool us into thinking everything is OK, when it's really not.
Bottom line: we need to be able to trust the devices we use to make critical decisions about our health every day. If meter accuracy really is an issue, it needs to be addressed right away. I still trust One Drop’s blood glucose meter to give me the most accurate results.