It’s no secret that managing your weight is an important part of any self-care routine, nor is it news that obesity can lead to a number of health issues, including diabetes. In fact, it’s estimated that obesity may account for up to 80% of cases of type 2 diabetes. But, considering all of the other factors that can affect your risk of diabetes—from ethnicity and genetics to lifestyle factors that have nothing to do with weight—why is the association between obesity and diabetes so strong?
First, Let’s Define “Obesity”
In the simplest terms, obesity is a condition characterized by an excess amount of body fat, which can increase the risk of not only diabetes, but also high blood pressure, certain cancers, and heart disease.
Body mass index (BMI), which calculates your weight-to-height ratio, is typically used to screen for obesity. Your BMI can fall into one of four weight categories: healthy (18.5-24.9), underweight (>18.5), overweight (25-29.9), or obese (>30).
However, BMI is notoriously flawed (for one thing, the formula was created centuries ago by a mathematician, not a doctor or other health expert), and while it may be used as one of the first steps in screening for and potentially diagnosing obesity, the number can only tell you so much about your health. That’s why it’s important to use alternative metrics, such as waist circumference and body fat percentage, to get a more well-rounded perspective of your health and your risk of any issues down the road. (Learn more about BMI and BMI alternatives here.)
Now, before we dive into the relationship between obesity and diabetes, it’s worth noting again that excess weight is just one of several possible risk factors for diabetes, from age, race, and family history, to high blood pressure and high cholesterol.
In other words: "Keep in mind that when something raises your risk for a certain condition, it does not mean that you will absolutely experience that condition,” says One Drop coach, Julia Dugas, a registered dietitian/nutritionist (RDN) and certified personal trainer (CPT).
How Are Obesity and Diabetes Connected?
One theory behind the relationship between obesity and diabetes is very simple: If more calories are coming into your body than are going out, you’re probably going to gain weight and potentially increase your risk of obesity and, in turn, diabetes. Thanks to the huge increase in the prevalence of processed foods in our culture over the last few decades, not to mention the sedentary lifestyles associated with most 9-5 jobs, many of us do consume more calories than we burn.
However, the calories-in-calories-out theory doesn’t give us the entire picture. It leaves one major question unanswered: Why do our fat cells hold onto these calories instead of releasing them as energy for our bodies?
In a recent paper published in the American Journal of Clinical Nutrition, public health experts, scientists, and researchers argued that obesity isn’t just caused by an imbalance of calories taken in vs. calories going out, but also by the way those calories impact our body’s production of the hormone insulin. Insulin is responsible for moving sugar from our blood and into our cells where it can be used for energy. When we eat a lot of processed carbohydrates, including concentrated sugar and refined grains, our pancreas releases considerable amounts of insulin. Over time, our cells may develop insulin resistance, meaning the cells will have a tougher time using glucose for energy. The pancreas then responds by increasing the production of insulin until it eventually fatigues and is unable to produce enough insulin to effectively clear sugars from the blood. The result: higher blood sugar and, in turn, a higher risk of diabetes.
That said, excess weight alone doesn’t definitively determine whether you’ll experience more or less insulin resistance (or, for that matter, a higher or lower risk of diabetes). Where you carry that extra weight can affect your risk as well, particularly if you’re carrying it around vital organs in the abdomen, says One Drop coach, Alexa Stelzer, RDN, certified diabetes care and education specialist (CDCES).
“Gaining excess weight around the abdomen releases pro-inflammatory chemicals that can lead to a less-sensitive insulin response,” explains Dr. Mubashar Rehman, PhD, PharmD, an assistant professor of pharmaceutical sciences at Quaid-i-Azam University in Pakistan.
But it’s not just that weight gain can lead to insulin resistance and, possibly, diabetes. “It’s also true that insulin resistance can occur prior to obesity and actually be a cause of weight gain,” says Stelzer. “Insulin resistance can signal the body to convert extra energy to be stored as fat around organs and muscles.”
Managing Obesity and Diabetes
Considering the many ways diabetes and obesity are connected, you’ll find some overlap in managing the two conditions as well.
For both obesity and diabetes, healthy eating and regular exercise are self-care staples. In terms of nutrition, One Drop coach, Lindsay Vettleson, RDN, CDCES, CPT recommends that you not only incorporate fresh fruits and vegetables as much as possible but that you also include a variety of whole foods in your day-to-day meals to ensure you’re getting a good balance of fiber, protein, healthy fats, and other important nutrients. (Need help figuring out which foods to shop for? Check out our beginner’s guide to heart-healthy eating and our tips on plant-based nutrition.)
As for exercise, the American Diabetes Association (ADA)’s Standards of Medical Care state that most adults with diabetes (both type 1 and type 2) should engage in 150 minutes or more of moderate- (e.g., brisk walking, light bicycling) to vigorous-intensity (e.g., hiking, jogging) aerobic activity per week, spread over at least three days per week, with no more than two consecutive days without activity. The ADA’s guidelines also say it’s a good idea to factor in two or three sessions of resistance exercise (and flexibility/balance training for older adults with diabetes) per week, and, of course, limit the time you spend sitting as much as possible (translation: try to get up and move around a little every half hour or so).
Official recommendations aside, be sure to create a routine you actually like and look forward to executing, notes Dugas. “If we aren’t choosing exercise methods we enjoy, the chance we’ll stick with them long-term is unlikely,” she explains. Whether you love strength training and walking, running and pilates, or even chair yoga and taking the stairs in lieu of the elevator when you can, “choose the path of least resistance if you really want to stick with an exercise program,” says Dugas.
As important as nutrition and exercise are, though, they’re not everything. It’s also crucial to manage your stress levels, as your body’s stress response triggers the release of several hormones that can spike your blood sugar and, when left unchecked over time, can lead to chronically high blood sugar levels, explains Vettleson.
Plus, “stress can lead to stress eating,” adds Dugas. “Eating when we aren’t physically hungry won’t benefit us in the long run, so instead, we should be looking inward,” she explains. “What are we feeling in those moments when we reach for food, but aren’t hungry? What was the trigger that led us to the fridge or pantry? What would a more productive activity be than eating to actually help reduce stress? Perhaps a walk, a conversation with a friend, curling up with a good book, or working with a therapist to develop coping skills?” (Explore more ways to handle stress and emotional eating.)
Even chronic sleep deprivation and poor-quality rest can have a similar effect on the body to stress, notes Vettleson. Inadequate sleep can spike your body’s production of the stress hormone cortisol—which we already know can lead to increased insulin resistance and higher blood sugar levels—and it can disturb your appetite hormones, making you feel hungrier and less satisfied when you do eat. (Here’s how to sleep well for healthy blood sugar levels, plus ways to improve your nutrition for better sleep and blood sugar.)
Of course, these types of lifestyle changes might only take you so far. Whether it’s to manage obesity, diabetes, or both, some people do benefit from adding medication to their regimen, too. If you live with obesity, your doctor may prescribe you a weight-loss medication, or, depending on your situation, sometimes surgery and other medical procedures are needed as well.
As for diabetes, medication needs depend on quite a few different factors, including the type of diabetes you have, your level of insulin resistance, and more. (Learn more about diabetes medication here.)
Regardless of whether or not you’ll need medication or surgery to manage obesity and diabetes, all of these approaches are meant to be coupled with lasting lifestyle changes. That means finding out how you personally stay motivated to take care of yourself every day, devising problem-solving strategies to maintain your progress, and getting support from people with similar goals and challenges, says Vettleson.
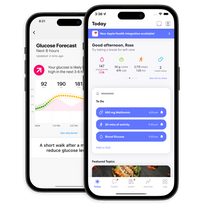
To start making those lifestyle changes into lifelong habits, become a One Drop Premium member and work with one of our certified health coaches on your goals, roadblocks, and everything in between.
This article has been clinically reviewed by Alexa Stelzer, RDN, CDCES, clinical health coach at One Drop, and Jamillah Hoy-Rosas, MPH, RDN, CDCES, and VP of clinical operations at One Drop.