Read time: 6 minutes
- When you live with a chronic condition, treatment-related burnout can leave you feeling mentally, physically, and emotionally exhausted by the ongoing stress of managing your health.
- Dealing with treatment-related burnout means zeroing in on what causes your stress to become unmanageable, whether it’s perfectionism or lack of support or motivation.
- Burnout is inevitable, but that doesn’t mean it always has to overwhelm you.
Burnout is a chronic state characterized by physical, mental, and emotional exhaustion that happens when long-term stress curtails your energy and mental resources. Much like how a job can drain your energy and cause occupational burnout, managing a chronic condition can feel like a full-time job unto itself and can lead to treatment fatigue, also known as treatment-related burnout.
Burning Multiple Candles at All Ends
Let’s say you live with diabetes. When you’re first diagnosed, you’re hit with a lot of new information all at once: You have to learn how to use different medical devices, like a glucose meter or insulin pump; you’re tasked with rethinking your food and exercise habits; your doctor might ask you to change your approach to managing your weight; you may even have a laundry list of new medications to take. In fact, research shows that, on average, living with diabetes can require you to make an additional 180 decisions per day, solely about your health and self-care.
Eventually, of course, you get used to these new routines and the responsibility of making so many decisions each day. But, whatever your circumstances are, dealing with any chronic condition can take a huge toll on you, both mentally and physically. It demands your energy and attention every day, multiple times per day, and no matter how much work you put into it, you still might not be satisfied with your progress sometimes.
Once you’re a year, five years, or even decades into living with a chronic condition, it’s easy to wonder to yourself: If I haven’t “mastered” how to live with this by now, when will I? Will I ever “master” it? What’s the point of all of my effort?
Considering the psychological weight of that mental, emotional, and physical exhaustion, it makes sense that living with a chronic condition is associated with a two-fold higher chance of developing depression—odds that could increase your likelihood of missing work, dropping the ball on a passion project or two, becoming irritable around your loved ones, or even neglecting to take care of your health.
Now, compound the treatment-related burnout with any other type of burnout you might be experiencing, whether it’s coming from work, your personal life, or all of the above. That combination of burnout can accelerate the development of those depressive symptoms, potentially causing feelings of cynicism, apathy, and a sense that you aren’t successful with your work, personal life, or self-care, no matter how much effort and energy you exert into any of these areas.
Then, of course, you have the stress of the ongoing COVID-19 pandemic. Between the increased risk of COVID-related complications associated with chronic conditions, the isolation that comes with quarantining, and the many uncertainties that the pandemic has brought into the workplace—from the availability of employment opportunities (and the health insurance they provide) to safety concerns in high-risk job settings—burnout can come from countless different sources these days.
What Ignites the Flames of Burnout?
The truth is that burnout is inevitable when living with a chronic condition; you’re likely going to deal with peaks and valleys of treatment-related burnout throughout your life.
However, the exact causes won’t always be the same, and it’s important to home in on where those roots come from so you know how to address them and relieve your stress.
- Sometimes, the constant list of to-dos for your chronic condition will simply overwhelm your time, abilities, and energy on top of all of the other daily responsibilities of life, work, relationships, and more.
- Healthtech can certainly make your self-care easier, but there’s no denying the device fatigue that can come with it at times, from continuous glucose monitor (CGM) alarms to the eye strain of looking at too many screens.
- If you take a perfectionist approach to chronic condition management, that desire to do everything “perfectly” all the time will ultimately burn you out when you realize “perfection” doesn’t actually yield results.
- Even if you’re seeing progress in your health, a lack of positive feedback can mean a loss of satisfaction and motivation, and the feeling that engaging in healthy self-care practices is pointless.
- Your doctor may be setting high standards for you to achieve your health goals—for example, lose a certain amount of weight over a specific period of time—but they’re not necessarily giving you the day-to-day support needed to see those results, which could leave you feeling overwhelmed or powerless.
- Managing a chronic condition can bring enough stress upon you as it is, but everyone deals with relationship and family issues to some extent, too. Whether it’s the loss of a loved one or an ongoing family conflict, these life events can take the energy you might otherwise put toward your self-care, or make you feel that your chronic condition is a burden on the people you love.
Soothing the Burn(out)
Burnout may be unavoidable from time to time, but that doesn’t mean it’s impossible to manage. There are several steps you can take to better understand your experience with treatment-related burnout and reroute the direction it may be taking you in.
- Know how to identify the signs of burnout and when to ask for help. Before burnout usually comes psychological distress, or negative emotional experiences resulting from the challenge of managing your chronic condition. To measure that level of distress and understand just how much it may be affecting you, consider using condition-specific distress-screening tools. The Diabetes Distress Scale (DDS), for example, is a free online resource that can help you see the warning signs of burnout and know when to seek clinical help. If it turns out that you’re interested in working with a therapist, check out the American Diabetes Association (ADA)’s mental health provider directory, Psychology Today’s website, or mentalhealth.gov to find an expert near you.
- Practice self-compassion. Self-compassion doesn’t just mean speaking to yourself the same way you would to a loved one in distress. It also means acknowledging your humanity and the imperfections that come with managing an imperfect chronic condition. It’s about accepting that there is no “mastery” of your condition, and redirecting your focus from one of “perfection” to one of growth, progress, and the pursuit of healthy ways to manage and negotiate each decision as you confront them.
- Surround yourself with people who recognize your hard work. It’s one thing to show yourself love and compassion, but it’s still valuable to get that validation from others as well. Maybe it’s a co-worker who relates to your experience with burnout, someone you hit it off with at a waiting room during a doctor’s appointment, or even your One Drop health coach. Whoever’s in your corner, make sure they make you feel uplifted and empowered in your self-care habits.
- Become an advocate for your chronic condition—or anything else you’re passionate about. Maybe you want to help organize group support meetings for people living with diabetes in your area, or perhaps you’re interested in using your athletic abilities to bring affordable workout classes to people in your town who can’t afford gym memberships. Whatever makes you feel driven and motivated, advocating for a cause you care about can give you a sense of purpose outside of the day-to-day responsibilities of your chronic condition, your job, your relationships with loved ones, and everything else in life. Advocacy can help empower you when you may be feeling powerless in these other aspects of your life.
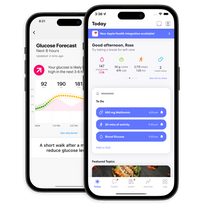
- Harness the power of behavioral data science. Combining the human-centered approach of behavioral sciences like psychology with that of computer-focused fields like data science and artificial intelligence, behavioral data science brings a holistic perspective to chronic condition management. Data science techniques can power health predictions and insights that simplify daily decision-making, while personalized health coaching eases the cognitive burden of treatment-related burnout and provides positive reinforcement to keep you motivated. To see what else behavioral data science can offer you, become a One Drop Premium member and show burnout who’s boss.